
Taranaki GPs in the latest RNZCGP workforce survey were the LEAST likely to recommend General Practice as a career with net promoter score of -20.
Trekking around Pinnacle MHN practices in the region with business development mangager and network leader Pauline Cruikshank and new GP Liaison and Auckland University Academic C0-ordinator Nadja Gottfert over the last few days it was really hard to match this fact with the enthusiasm and innovation that the GPs displayed.

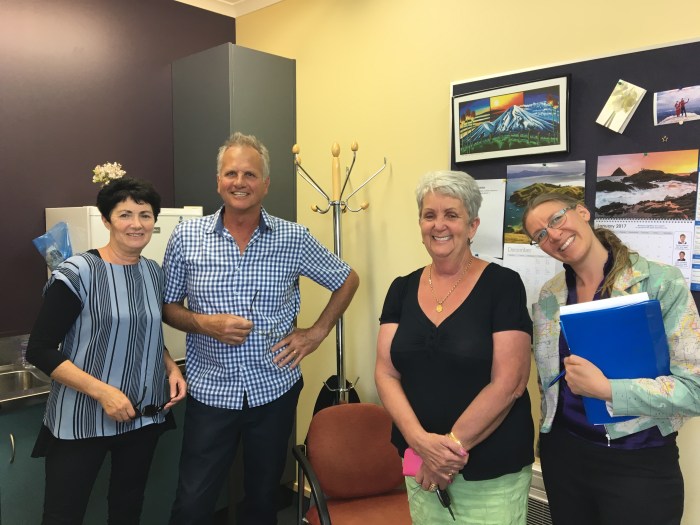
At Inglewood Medical Centre we met Marie Fonseka, Cees Dekker and Steve Finnigan ( second from the left) – the FIRST GP to put his hand up for moving to the new PMS system INDICI which will create opportunities for true patient centred electronic medical records and an ability to integrate care across the whole of the health and social sector.

At Eltham Health Centre we met Anton Westraad – a solo GP who has championed insulin initiation in rural practices – preventing patients from having to travel an hour to Base hospital to meet with a specialist nurse. Anton’s work has been supported by Pinnacle’s Primary Options funding to keep patients close to home when they have issues like cellulitis, DVT , pneumonia, or needing rehydration after gastroenteritis.
Gerard Radich and his wife Margot run a solo general practice in Stratford – his dedication to his patients is phenomenal – everyone is informed of every test result, he answers the phones at morning tea time so his staff can have a break – an early demonstration of the benefits of the Health Care Home GP phone triage he finds he can deal with most patients who call during this time without needing a face to face consultation.

At Patea and District Community Medical trust we saw fantastic leadership in practice manager Christine Steiner who steers a practice in a very high needs community on the edge of the region in a small coastal town two hours away from Base hospital. The regular doctor Maria Beltran De Guervara was away on holiday when we visited but they provide PRIME services and the nurses truly work at the peak of their scope. 
Karen Caskey ( Practice manager) Duncan Burns, Bill Carteledge, and Brian Wood at Avon Medical Centre are implementing the Health Care Home model of care, enthusiastic teachers with 2 RNZCGP registrars booked to learn alongside them in 2017.

GP educator and ex-GP liaison Dr Viv Law of the Family Health Centre in New Plymouth runs the Taranaki Medical Foundation which Pinnacle supports to provide GPs with regular high quality education events in the region.
And we saw LOTS of Christmas Trees !!



( Our Favourite !!) Thanks to Ngati Ruanui Health Care.
So why the low “net promoter”score?
In a meeting with Taranaki CEO Rosemary Clements a group of GPs identified the pressures (and pleasures) of being a solo GP – maybe the need to be “bum up nose down”all the time seeing patients makes them less likely to recommend GP as a career.
The financial pressures on General Practice are worsening year on year – small rural practices really feel the pinch especially if they are Very Low Cost Access and the paperwork involved in managing a practice and compliance costs of meeting regulations and accreditation continue to escalate.
The solution may be to increase the number of training positions in the region for undergraduate and post-graduate doctors and nurses.
Enabling more to be done more simply in primary care through near patient testing and better management of patients as they approach end of life through advanced care planning.
The GP’s in the region discussed the need to change the business model and to look for other sources of funding outside of vote health.
They focused on the need to maintain the current aging work force to be happy and competent for as long as possible so that they as clinicians stay in position whilst new providers are in the pipeline. They also said they wanted a whole system approach to managing patients and look forward to better integration of care across primary and secondary sectors as promised by the Health Action Plan.
Pinnacle’s Mission is to get the best health outcomes for people and their communities and do this by supporting general practice to deliver high quality care.
We are collaborative, adaptive, aware, reliable, innovative, inquisitive, courageous and keen to help !
Dr Jo Scott-Jones ( Medical Director) and Nadja Gottfert (GP Liaison and GP Academic)













