The topic of “wheeze” can get very complicated with different approaches needed for adults and children, and different conditions overlapping and changing as a person’s life progresses.
This article links to several resources available and hopefully helps GPs manage the muddle.
Asthma is an illness that is frequently coded in encounters by GPs – and guidelines are pretty straightforward – but this is an area where practices may need to decide on a consistent approach to care.
Under the guidance of the MOH and the new “system level milestones” plan the combined DHBs of Midlands have challenged GPs in the region to reduce admissions for children aged 0-4 years and they have put a particular focus on respiratory disease.
One of our problems looking at the topic is the difference between “wheeze” – the polyphonic high pitched expiratory noise made by restricted airways, “asthma” the hyperresonsiveness of airways characterised by constriction of smooth muscle, and inflammation and COPD the decrease in airway patency that develops over time and linked to permanent reduction in lung function.
It’s important to remember, the majority of children who wheeze in the first few years of life will “grow out” of the condition.
And interesting to note that around 40% of people with COPD also have asthma.
Prevalence: Let’s look at asthma….
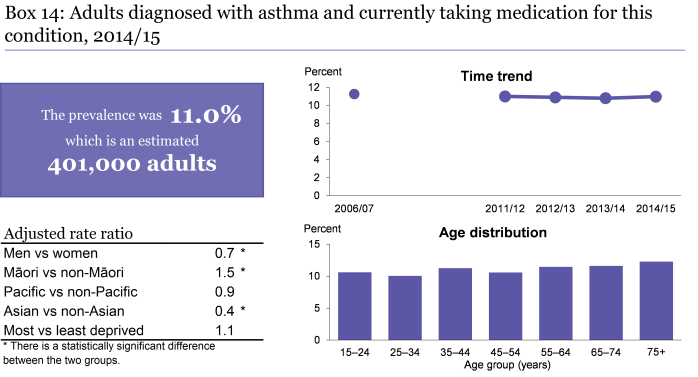
The latest NZ Health Survey tells us that 11% of NZ’ers and 15% of Maori aged 15 yrs or over are using asthma medications.
Issues:
The Health Quality and Safety Commission tell us that in adults:
- 82 percent people admitted with asthma did not receive a paid for influenza vaccine in the year after admission. People with asthma should have an annual flu vaccine.
- Over a third of people admitted with asthma were not regularly given asthma controller inhalers (brown, inhaled corticosteroid) in the year after their admission.
- In the community, 30 percent of asthmatics regularly dispensed relievers were not regularly dispensed a controller.
- Admissions for Pacific people and Māori are proportionally higher at all ages than those identifying as European or Other.
They also note young children are much more likely to be admitted to hospital for “asthma” than older children (10 – 14 years) and adults.
HSQC illustrate significant variation from one DHB to another – for example across 4 Midlands DHBs the rate of admissions of children aged 0-4 with asthma or wheeze is shown below:
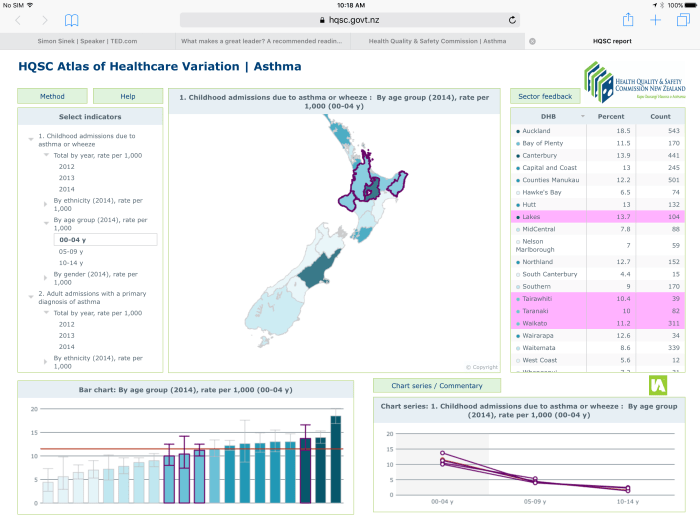
Why do some DHBs have a lower or higher rate than the national mean ? Does this reflect differences in population or are there other factors?
What can be done to reduce admission to hospital / ED attendance for children with wheeze?
DHB variation:
These DHBs do have some differences in their population make up – but does this explain anything? Is there something special about Lakes that mean the rates of admission is higher? Is it a significant difference?
Is it an environmental issue ? Does it relate to access to services or a different burden of illness?
We don’t know if this something in our control as GPs but it is interesting to note and worth thinking about.
Why do people take their children to ED with wheeze?
Studies suggest that in total only around 11% of use of ED is “inappropriate” .
Preventing patients self-referring with low urgency problems that are unlikely to require admission and are more suitable for other services, such as primary care, telephone advice helplines or pharmacy is a health promotion activity best targeted at parents of young children and at older youths/young adults.
The issues are greatest during weekends and bank holidays and service provision focusing on access to primary care and having urgent care services in the most deprived communities would have the most benefit as would the improvement of parental confidence.
Parents of children with acute breathing difficulties need those children assessed – and if we are going to have an impact we are either going to need to provide alternative care in the community away from ED that patients will access, or we need to reduce the number of children with respiratory problems.
Preventing the development of asthma itself is in the too hard basket and until we really understand the causes issues like the “hygiene hypothesis” and prenatal allergen exposure will remain in a dusty corner of the kete.
Exclusive breast feeding in the first few months after birth is associated with a reduction in incidence of asthma, and we do know there is an increase in wheezing illness in children on whole cow’s milk and soy based milk products.
Exposure to tobacco smoke pre and post-natally is associated with increased wheezing illness in childhood so our efforts to reduce smoking are important.
The key for GPs is going to be in the effective use of treatment for wheeze in children.
As a foundation we all need to develop and maintain good communication with families so that we can provide good quality education and improve concurrence with evidence based advice.
We need to see parental education as a key part of our role as GPs – teaching people what to do when they are worried and showing them what they really need to worry about, and what they don’t need to worry about.
We then need to be there for our patients – if we cannot provide a 24 hr a day service ourselves we need to show our patients how to access helplines and after hours services that are appropriate to their needs.
The next building block is to be actively engaged in whatever prevention actions that we know will help.
We can help identify and reduce exposure to risk factors – allergens and pollutants both indoor and outdoor, identifying the rare child with food allergy, avoiding using aspirin and NSAIDS, and help weight control.
We can provide effective treatment of rhinitis, sinusitis, and nasal polyps – this all helps reduce “wheeze” episodes in children.
We forget how important immunisation is sometimes – because we have acheived such a high uptake in our communities – but recent upsurges in pertussis remind us of how important it is that we keep working on this.
Finally we need to provide the best treatment possible.
For younger children the Best Practice Advisory Center tell us that not all that wheezes is asthma in children and their pragmatic approach to symptom management and prevention is great advice.
For older children we need to assess, treat and monitor asthma carefully.
We need to give patients an easy way to assess their own asthma control – using simple questionnaires (even though it is Pharma supported the Asthma Control Test is a good one) or for those capable of using them PEFR guidelines .
We need to take an evidence based and comprehensive approach to managing asthma – stepping up if symptoms are worsening, reviewing and intervening effectively after an exacerbation, and stepping down if appropriate.
Where do you find the evidence to help you decide what to do ?
Health Navigator is a great NZ resource to review with great information for patients and professionals – they have a great series of videos talking about how to use inhaler’s properly and what can trigger asthma for patients to view.
Internationally the National Institute for Health and Care Excellence ( NICE ) gives a detailed and up to date evidence and management guidance around a range of conditions.
Have a look at their pathway on bronchiolitis in children – those of you familiar with “maps” will recognise the algorithm based decision support tool, the layout and windows here are very user friendly.
Any review of guidelines is worth tempering with a health dose of skepticism from the Therapeutics Education Collaboration if you don’t link to their podcasts and look at the website regularly already make it an early “go to” when you are looking for an update on clinical issues.
The “search” facility doesn’t pull up a lot on childhood wheeze but there’s a bit on asthma and they do link to this interesting COPD tool that shows you your “lung age.”
They also link to Tools for Practice which is another great #FOAM4GP resource that shares the Evidence Based Medicine expertise of the Alberta College of Family Practice internationally.
Combining a scan of all these sites should give you good answers to clinical questions with the latest and best evidence available for example –
In asthmatics, LABA should not be used without inhaled steroids. LABAs increase serious adverse events when used alone, but not when combined with an inhaled steroid (at least in patients >12 years-old). The evidence for benefit of adding in a LABA is very small which is why they are best added in to patients who have significant symptoms despite other therapy.
LABA monotherapy does not increase adverse events in COPD patients and statistically significantly reduces the risk of COPD exacerbations requiring hospitalization (NNT=56)
Unanswered questions :
What would be the impact of using a regular ICS on admission to hospital / ED attendance for someone with poorly controlled asthma?
Studies suggest this might lead to a 55% reduction in severe exacerbations of asthma.
What would be the impact of flu vaccination on admission to hospital / ED attendence for people with asthma or COPD?
There is doubt about whether or not flu vaccine helps to reduce asthma exacerbations, but the benefits of flu vaccine across a wide range of parameters including reducing admissions with flu related complications is strong.
