March 2025
Clinical Snippets March 2025
1. Prescribing Testosterone
(i) A 2024 BPAC article on prescribing testosterone in aging males noted approximately 0.3% of males in New Zealand were dispensed testosterone in 2023, and use is increasing each year. In 2023, 6,620 males were dispensed testosterone compared to 4,815 in 2018; a 37% increase. The largest group of males dispensed testosterone was aged between 50 and 69 years, but increases in dispensing rates occurred across all age groups during this period, most notably in the 20 to 29 years age group (120% increase) and 30 to 39 years age group (80% increase).
(ii) The BPAC article gives a comprehensive review of diagnosis and management of testosterone deficiency in the older male including a very handy management flow chart. Relevant information is also summarised in the Health Pathways topic Testosterone Deficiency in Men. The importance of discussing potential adverse effects, monitoring requirements, the uncertain long-term risks and need for life-long treatment is emphasised. Other key practice points include:
- Investigation of testosterone levels (and consideration for treatment) is only indicated in patients with specific symptoms of hypogonadism that are impacting their quality of life, e.g. decreased libido and sexual function
- Hypogonadism is diagnosed based on at least two early morning serum total testosterone levels below the accepted threshold of normal in a patient with multiple features consistent with low testosterone. If low testosterone is detected, first identify and address any modifiable causes
- A six-month trial of testosterone is recommended; if there is no benefit at six months, treatment should be stopped. N.B. Maximal therapeutic effect may not be obtained until 12 months of treatment. Most patients can be initiated on daily transdermal testosterone gel as it allows dose modification and abrupt withdrawal, if required
(iii) A recent Research Review Conference Review reported on the 2024 T4L Testosterone Therapy and Men’s Health Congress contains summaries of the latest research on many aspects of testosterone deficiency diagnosis and management and is well worth a read for those interested. Our local endocrinologist Dr Ryan Paul introduces the summary and includes some interesting points including:
- There is no ‘andropause’ or ‘manopause’; rather, testosterone levels only reduce by approximately 1% per year in healthy men. The reason as to why testosterone deficiency is so prevalent with advancing age worldwide is due to many factors, especially obesity, diabetes and other chronic illness (suppresses HPG axis). In these men, treatment of the underlying cause, rather than testosterone replacement, is typically always the preferred option if possible.
- The prevalence of testosterone deficiency is also increasing worldwide due to the suppression of the HPG axis from either misuse of androgens (e.g. athletes, body builders) or inappropriately prescribed testosterone supplementation, which is why choosing appropriate candidates for testosterone replacement is more important than ever.
- Despite agreement regarding treatment of symptomatic men with confirmed hypogonadism, there continues to be no clear consensus on the treatment of asymptomatic men with confirmed hypogonadism, or symptomatic men with low normal testosterone levels. The measurement of free testosterone can be helpful in the latter group. However, it is important to know that unlike other countries, total testosterone and SHBG are usually measured in Aotearoa NZ by immunoassay, and not by mass spectrometry. Bothof these immunoassays are relatively inaccurate in the lower range, which is the most common scenario in diabetes and or obesity. As a result, indirect calculations of free testosterone are often inaccurate, and this is why some laboratories choose not to report them.
(iv) One of the latest Tools for Practice gems (#376 – Testosterone supplementation for cis-gender men: Let’s (andro-)pause for a moment) examined the clinical question What are the benefits and harms of testosterone supplementation in healthy cis-gender men or those with age-related low testosterone? The bottom line was that compared to placebo, testosterone may increase lean body mass by ~1.6kg in older men but has no consistent, meaningful impact on sexual function, strength, fatigue, or cognition. Testosterone does not increase prostate events, myocardial infarction or stroke, but pulmonary embolism (0.9% versus 0.5% placebo) and atrial fibrillation (3.5% versus 2.4% placebo) may be increased. Canadian guidelines note exogeneous testosterone therapy can impair male fertility due to decreased sperm production.
(v) Advice on switching between IM and transdermal preparations is available in a NHS resource although not all preparations listed in the handout are available in NZ.
2. Medical Tourism and ACC Treatment Injury Cover
With an increasing number of patients travelling overseas for surgical procedures such as bariatric surgery, various cosmetic procedures and dental work, the question is sometimes asked whether these patients might be eligible for ACC Treatment injury cover if they experience complications on return to New Zealand. The short answer is ‘it depends’. According to business rules released under the OIA, a personal injury caused by a treatment injury to a person at an overseas location must receive an accepted cover decision only if all of the following are true:
- the personal injury meets the criteria for acceptance of cover for all of the following:
- a personal injury
- the date of the treatment [causing the treatment injury] is on or after 1 July 2005
- the treatment [causing the treatment injury] occurred at a location not in New Zealand
- the overseas health care provider [causing that treatment injury] was not a New Zealand registered health professional on the date that treatment was provided
- the person that received the treatment [causing the treatment injury] was ordinarily resident in New Zealand on the date on which that treatment occurred
- the treatment [causing the treatment injury] was within the scope of practice of the overseas health care provider providing that treatment
- that overseas health care provider holds qualifications within that scope of practice
- there is a registration authority for that scope of practice in New Zealand
- that registration authority confirms those qualifications as being equivalent to New Zealand qualifications for that scope of practice
- the overseas health care provider [causing the treatment injury] holds a practising certificate that meets the criteria for being a valid overseas practising certificate for that treatment provider
There is considerable ‘devil in the detail’ regarding assessment of the provider’s qualifications and scope of practice, validity of their practicing certificate, and whether treatment occurred in a ‘comparable’ (for medical treatment) overseas country (quite a limited list which doesn’t include Thailand, India or Mexico).
3. Patient access to their clinical records
The Medical Council of New Zealand has responded to frequently asked questions about patients requesting copies of their medical records, in line with Rule 6 of the Health Information Privacy Code:
- Patients have the right to access their health information, regardless of the reason.
- Practices should be guided by the patient’s preference as to the format of the copy of their record, i.e. electronic or hard copy, however: discuss the potential risks of a hard copy, e.g. more likely to be lost, misplaced or accessed by someone unintended compared to electronic records. Raising awareness of possible risks can help patients to make an informed decision about how they would like to receive their records.
- Patients cannot generally be charged by practices (health agencies) for providing their medical records (including hard copies), unless:
- the patient has requested the same information within the past 12 months; or
- the request involves making copies of X-rays, video recordings, MRI scans, PET scans, or CAT scans due to the associated costs.
- If the charge is likely to exceed $30, you need to give the person an estimate of the charge before dealing with the request. You can request the payment be made before you provide the information to the person.
4. Equity – dementia treatment
The February issue of GP Voice included a well referenced article by a local psychiatrist on primary care challenges in managing dementia including inequitable access to memory clinics and non-pharmacological interventions for dementia management. The article notes that donepezil has been Pharmac-funded since 2010, and has demonstrated cost-effectiveness in both mild-to-moderate and moderate-to-severe Alzheimer’s disease.
The author notes prescription data reveals concerning patterns. Between 2016 and 2020, only one-third of Aotearoa New Zealand’s dementia population received funded anti-dementia medication, compared to over half in the UK. Māori and Pasifika were prescribed these medications at lower rates than those of European ethnicity, mirroring similar inequities observed among lower socioeconomic and rural populations in Australia. This is despite Māori and Pasifika typically presenting with dementia at younger ages than New Zealand Europeans, with Pasifika often presenting at more advanced stages.
A small survey (43) of GPs undertaken via e-Pulse found that close to half the respondents prescribed donepezil to less than 25 percent of diagnosed patients. Primary reasons for not prescribing donepezil included perceived poor efficacy, side effect concerns and lack of confidence or experience.
The author concluded: the low prescription rate of anti-dementia medications in Aotearoa New Zealand appears primarily driven by limited discussion of pharmacological options in primary care settings. This constraint potentially undermines patient and family involvement in treatment decisions. While global attention focuses on novel, costly disease-modifying treatments, Aotearoa New Zealand must review its approach to established interventions to ensure equitable and effective dementia care.
A reminder that Health Pathways has a specific section on cholinesterase inhibitors including pre-prescribing assessment (Cognitive Impairment pathway) and planning, actual prescribing and reviewing response including deprescribing and medication switching advice.
5. Equity Good News
Issue 229 of Respiratory Research Review reported a recently published article on patterns of asthma medication use and hospital discharges in Māori in Aotearoa New Zealand. The researchers found that from 2019 to 2023, there were relative increases in budesonide-formoterol dispensing of 111% for Māori and 115% for non-Māori, and that asthma hospital discharges fell 32% from 142.5 to 97.3 per 100,000 for Māori and 23% from 49.4 to 37.9 for non-Māori. The reviewer noted the increase in ICS/formoterol for maintenance and reliever therapy and that prescriptions for SABAs has decreased in line with the NZ Guidelines but there is still some way to go to see asthma admission rates for Maori falling to those of non-Maori. To compare your asthma prescribing habits with your practice and national peers go to the He Ako Hiringa website and access your stats and an audit template through the Epic dashboard.
6. Prescriber Update
The March 2025 Prescriber Update includes a couple of timely reminders:
i) Weekly methotrexate key messages:
- Weekly methotrexate is indicated in adults for severe, recalcitrant disabling psoriasis and severe, recalcitrant active rheumatoid arthritis that are not responsive to other forms of therapy.
- Mistaken daily use may cause serious and sometimes life-threatening or fatal toxicity in many organ systems.
- When used for psoriasis and rheumatoid arthritis, check that patients, families and/or caregivers: understand that methotrexate is taken once weekly, on the same day each week; are aware of the signs and symptoms of methotrexate toxicity and advise them to seek medical advice immediately if they occur.
- Advise patients, family and/or caregivers to seek medical advice immediately if signs or symptoms of methotrexate toxicity occur, including sore throat, bruising, mouth ulcers, nausea, vomiting, abdominal discomfort, dark urine, shortness of breath or cough.
- If either partner is receiving methotrexate, pregnancy should be avoided and effective contraception used during treatment and after discontinuation (for at least 3 months after treatment for males and at least 6 months for females).
- Monitor blood count, liver and renal function throughout treatment.
(ii) Colchicine toxicity key messages:
- Colchicine has a narrow therapeutic index and the separation between therapeutic and toxic doses is not well defined. Colchicine toxicity has a high mortality rate. There is a latent period of 2 to 12 hours between colchicine overdose and the onset of gastrointestinal symptoms. Cardiotoxicity (increased troponin) may also develop at any time after ingestion and has a poor prognosis. Multisystem failure generally occurs 24 to 72 hours after overdose. There is no specific antidote.
- Renal and hepatic impairment, older age and certain medicines can increase colchicine plasma levels, resulting in toxic effects. Consider these factors when initiating and continuing patients on colchicine. If the patient’s creatinine clearance is:
- ≤50 mL/min – reduce the colchicine dose by half
- ≤10 mL/min – colchicine is contraindicated
- Early symptoms of colchicine toxicity include burning and rawness in the mouth and throat, followed by severe nausea, vomiting, abdominal pain and haemorrhagic diarrhoea. Educate patients on the early symptoms of colchicine toxicity. Advise them to stop colchicine immediately and seek medical advice if symptoms occur.
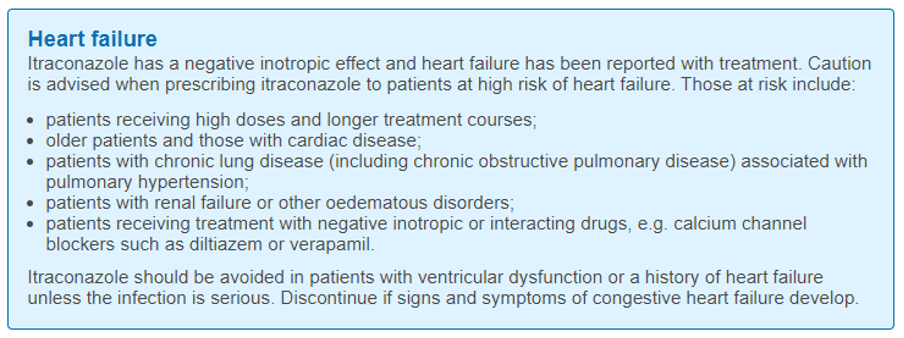
- Be aware of drug interactions that can cause increased colchicine plasma concentrations including: azole antifungals; macrolide antibiotics; calcium channel blockers diltiazem and verapamil; amiodarone; ciclosporin.
- Educate patients on safe storage and disposal to prevent paediatric exposure, which can be fatal.
7. Bits and Pieces
(i) BMJ Best Practice – After a successful trial period the health New Zealand Library is now subscribing to BMJ Best Practice long-term. By creating a user profile you can access the mobile app, CPD tracking and alerts. Primary care users can access the resource directly from the home page of your local health pathways website in order to set up a user profile.
(ii) Anaphylaxis –NZF is now listing an IV chlorpheniramine preparation under s 29 with the indication listed as emergency management of hypersensitivity. ANZCOR anaphylaxis guidance refers to consideration of oral antihistamine administration after standard emergency management with oxygen, IM adrenaline and IV fluids if required. IV or IM antihistamines are not generally recommended and particular caution is required if using parenteral promethazine. NZF notes intravenous administration of promethazine can cause severe tissue injury including gangrene; avoid extravasation. Only administer intravenously if no alternative—very slow administration of diluted injection solution via a large vein, and careful monitoring of the injection site, is required.
(iii) Pharmac has announced the progestogen only pill Cerazette (desogestrel) will be funded with no restrictions from 1 April 2025, so it can be prescribed for any relevant use. In addition to use for contraception, desogestrel can be used in the treatment of a range of conditions include endometriosis, premenstrual syndrome, polycystic ovary syndrome, heavy menstrual bleeding, period pain in adolescence, and for use as a part of menopausal hormone. For contraception desogestrel has a 12-hour window of use compared with the 3-hour window with current levonorgestrel and norethisterone preparations.
(iv) Coeliac disease: Following on from a 2022 article on diagnosis and management of coeliac disease, BPAC has published a primary care checklist for coeliac disease that includes brief summaries and algorithms of adult and pediatric diagnostic and management pathways and links to other resources available on the Coeliac NZ website.